(RxWiki News) Obesity and metabolic problems may not always go hand-in-hand. Some obese people may not develop the metabolic changes that are often tied to obesity.
A small study found that some people don’t develop metabolic changes that can precede heart disease, diabetes or stroke — even when they're obese. People who are obese often have metabolic abnormalities.
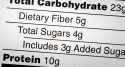
Among these are insulin resistance and high levels of cholesterol and other blood fats.
Even if they gained more weight during this study, some obese people who didn’t have metabolic problems when the study began did not develop them.
"This research demonstrates that some obese people are protected from the adverse metabolic effects of moderate weight gain, whereas others are predisposed to develop these problems," said lead study author Samuel Klein, MD, of the Washington University School of Medicine in St. Louis, in a press release.
“We need more studies to try to understand why obesity causes specific diseases in some people but not in others. Could it be genetics, specific dietary intake, physical lifestyle, emotional health or even the microbes that live in the gut?"
Insulin is a hormone that controls blood sugar. Developing insulin resistance can lead to type 2 diabetes — a risk factor for heart disease, stroke and kidney disease.
Some people who are obese, however, may not develop these metabolic problems. These patients, known as metabolically normal obese (MNO) people, have a much lower risk of developing diabetes and heart disease than others who are obese.
Dr. Klein and team wanted to know whether weight gain in MNO people could make them develop the metabolic abnormalities that precede diabetes and heart disease.
These researchers studied 20 people who had a body mass index (BMI) of about 36. BMI is a measure of body fat based on height and weight. A BMI of 30 or more is considered obese.
Twelve of the research subjects were MNO adults, and eight were metabolically abnormal obese (MAO) adults — meaning they developed the metabolic problems tied to obesity. These study subjects were about 43 years old and mostly female. All of these patients were healthy overall, did not smoke and did not take medications.
These patients chose all their meals from fast-food restaurants under the supervision of a dietitian over several months.
"Our goal was to have research participants consume 1,000 extra calories every day until each gained 6 percent of his or her body weight," said study author Elisa Fabbrini, MD, PhD, of Washington University.
The MNO patients appeared to be protected from the harmful effects of gaining too much weight, Dr. Klein and team found. For instance, the average fasting blood sugar in MNO patients rose from 93 to 96 milligrams per deciliter (mg/dl). In MAO patients, fasting blood sugar rose from 105 to 110 mg/dl.
In MAO patients, their average triglyceride reading rose from 134 mg/dl to 170 mg/dl. Triglycerides — blood fats tied to an increased risk of stroke — in MNO patients did not change.
The average blood pressure reading in MNO patients decreased from 123 over 67 to 118 over 67. Average blood pressure readings in MAO patients rose from 128 over 71 to 139 over 81. High blood pressure has been tied to an increased risk of heart disease and stroke.
At the end of this study, all of the patients entered a weight loss program and were helped to lose at least as much weight as they had gained during the study.
This study was published Jan. 2 in the Journal of Clinical Investigation.
Grants from the National Institutes of Health, the Central Society for Clinical and Translational Research, the Longer Life Foundation and the Kilo Foundation funded this research. The authors disclosed no conflicts of interest.