(RxWiki News) There's a small group of scientists very concerned about how the huge changes in what we put in our mouth over the last century has changed our guts.
The microscopic passengers we all carry around, those trillions and trillions of bacterial cells which outnumber us even in our own bodies, are probably not the same kinds of bacteria humans have co-existed with for the previous million years of evolution.
"Ask your doctor about fiber supplements and probiotics."
A small study from the University of Illinois, led by Kelly Swanson, PhD, showed that the amount and type of fiber present in food shifted the gut bacterial population from one kind to another.
While fiber is recommended for regulating bowel movements, that's not necessarily the only benefit.
There's some evidence that the kinds of things you eat, and how clean they are, affect your native population of bacteria. A high level of plant material can lead to an entirely different sort of situation in your colon than a diet heavy on meats and cheeses.
While a complicated topic, there is plenty of evidence linking poor colon health to some of the more mild forms of bowel irritation.
Daily fiber is recommended by doctors for the treatment of mild irritable bowel syndrome, and in addition to physically moving things along, the change in bacteria may play a role in helping with the symptoms.
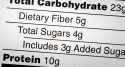
"When we understand what kinds of fiber best nurture these health-promoting bacteria, we should be able to modify imbalances to support and improve gastrointestinal health," Swanson said. "Unfortunately, people eat only about half of the 30 to 35 grams of daily fiber that is recommended."
The study looked at 20 men who were given 21 grams of corn fiber, no fiber, or 21 grams of a commercially made fiber product, polydextrose. Either type of fiber helped raise the overall level of bacteria in the intestine, especially the "friendly" bacterial groups.
The friendly bacteria that were shown to be increased by adding fiber were lactobacillus, commonly found in yogurt, and faecalibacterium, which has been shown to turn dietary fat into molecules that reduce inflammation.
Humans and the many types of bacteria, both friendly and dangerous, lead lives unknowingly dependent on one another. Several kinds of key vitamins, like Vitamin B12, are made by bacteria camping out in the intestinal tract, and are the only natural source.
The researchers took samples every day during a three week period, and analyzed the results from the three different treatments once the men in the study were finished with it. DNA sequencing matched the product with the kinds of bacteria present, and the percentage composition of each type.
Knowing how to raise the level of friendly bacteria is important, because overly aggressive treatment of patients with antibiotics can wipe out a lot of the friendly bacteria, which tend to be less well protected.
As a result, some health experts recommend stocking up on yogurt during antibiotic treatment to resupply your intestines with the good guys.
The study was published in the July 2012 edition of the Journal of Nutrition.
Research funding was provided in part by General Mills.